Legacy Consulting Services helps physicians, hospitals, and healthcare organizations across the nation manage provider enrollment, credentialing services, and recredentialing with precision, performance, and profitability. We streamline credentialing and enrollment so new physicians, therapists, and facilities can begin billing sooner.
Our credentialing experts manage all paperwork, payer follow-ups, and renewals, giving your team peace of mind and reducing revenue delays.
Fast, compliant credentialing solutions lead to faster payments and better cash flow.
Credentialing Done Right: Enroll with Payors, Start Billing Sooner
Provider credentialing (also called provider enrollment) is the process of completing and submitting applications with commercial insurance plans, Medicare, Medicaid, and Blue Cross Blue Shield (BCBS) so a healthcare provider can be approved, credentialed, and authorized to bill for services. This also involves verifying the provider’s qualifications, including licenses, education, board certifications, malpractice coverage, and work history, and maintaining active participation through recredentialing and CAQH/PECOS updates.
What is the benefit of credentialing services? In short, credentialing ensures compliance, builds patient trust, and protects your organization from reimbursement delays or compliance penalties.
Our Credentialing Services
Legacy’s team handles every stage of credentialing and enrollment, ensuring nothing falls through the cracks.
What’s Included
- New Provider Enrollment — Full professional credential services with commercial, Medicare, and Medicaid payors.
- Recredentialing / Maintenance — Track expirations, update CAQH, and renew credentials on schedule.
- Payor Network Enrollment — Add new payors or locations quickly, avoiding revenue interruptions.
- CAQH & PECOS Management — Create and maintain provider profiles, reducing administrative burden.
- Hospital Privileging — Coordinate provider files for hospital or facility privileges.
- Credentialing Audits — Identify gaps and clean up provider data for compliance.
What is The Real Cost of Credentialing Delays?
Many providers don't realize the true financial impact of delayed credentialing. Every day your provider isn't credentialed means lost revenue from unbilled claims.
Example: If a provider generates an average of $5,000 per day in billable services, a 30-day delay could mean a $150,000 loss in potential revenue. Can your practice afford to wait? Most payors don't give retroactive effective dates.
How the Credentialing Process Works
Step 1: Collect provider data and supporting documents
Step 2: Verify licenses, NPI, DEA, board certification, and work history
Step 3: Prepare and submit payor applications (Commercial, Medicare, Medicaid)
Step 4: Manage CAQH, PECOS, and state portals
Step 5: Follow up and track status to approval
Step 6: Confirm participation and effective date
Typical timeline: 60–120 days, depending on payor response time.
How Long Does Credentialing Take?
Credentialing timelines vary by payor, provider type, and state regulations. In many practices, delays extend well beyond 90 days — and those backlogs can cost thousands per provider monthly.
On average:
- Commercial payors: 90–120 days
- Medicare/Medicaid: 60–90 days
- Hospital privileging: 60–180 days
Tip: Missing documents or outdated CAQH profiles are the #1 cause of credentialing delays. Legacy prevents these issues by maintaining provider files proactively. Start the credentialing process early to avoid delays in accepting new patients and getting reimbursed for services.
Are credentialing services worth it? Yes — because faster credentialing means fewer denied claims, quicker billing, and more predictable revenue.
Requirements for Provider Enrollment
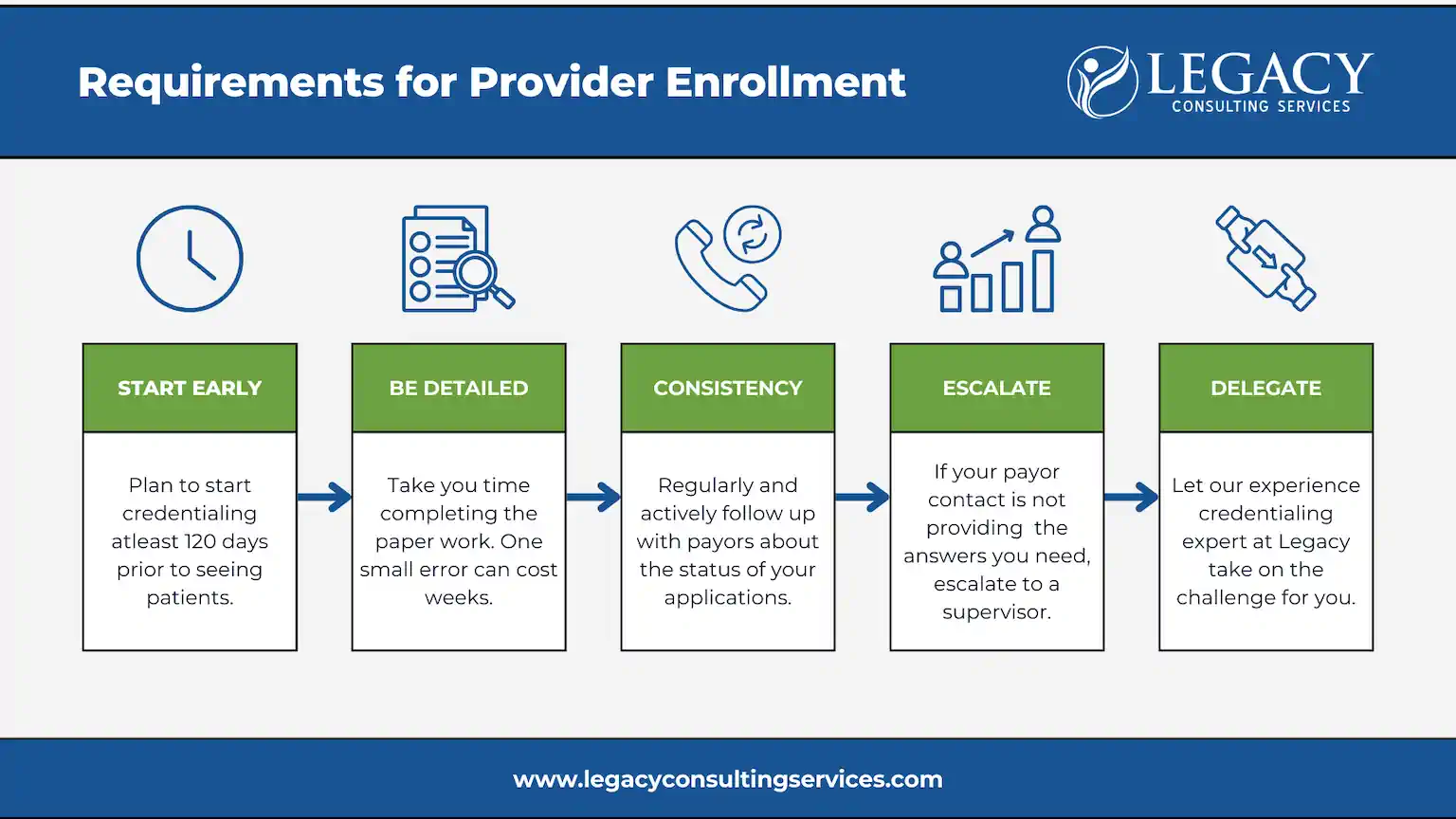
Specific requirements must be met for each provider and payer to ensure smooth and timely enrollment.
Why Outsource Credentialing to Legacy Consulting?
Unlike other credentialing services for providers that simply submit paperwork and wait, we take a proactive, hands-on approach to ensure your providers are credentialed and enrolled as quickly and smoothly as possible.
Waiting on credentialing approvals isn’t just frustrating — it often leads to lost revenue, increased denials, and unnecessary administrative burden. Outsourcing credentialing saves your team time, frustration, and lost revenue.
Here’s why providers trust us:
-
- Improved Cash Flow: With quicker enrollments, your practice can bill payors faster, preventing cash flow disruptions and ensuring steady revenue.
- Less Administrative Burden: We take credentialing off your plate, allowing your staff to focus on patient care and operations rather than paperwork.
- Speedy & Accurate Enrollment: We understand the attention to detail required for the credentialing process, ensuring faster approvals from insurers and minimizing delays.
- Experienced & Knowledgeable Team: Our experts are always up-to-date on the latest payer requirements and healthcare credentialing regulations.
- Stronger Payor Relationships: Our team's expertise in working with insurance companies ensures smoother interactions and better outcomes for your practice.
- Comprehensive Solutions: From CAQH registration to re-credentialing, we offer complete end-to-end credentialing services for your practice and providers. We also can streamline the approval process of Privileging & Hospital Appointments.
- Integrated approach: Our team also manages contracting, billing, and payor enrollment for seamless revenue cycle integration.
How much do people charge for credentialing? Pricing depends on the scope of services — from one-time provider enrollment to full-scale credentialing services pricing packages. Contact us for a tailored quote.
What are the three types of credentialing? Provider enrollment, recredentialing, and hospital privileging — all managed by Legacy’s credentialing specialists. Read a testimonial from one or more of our clients about how we expedited the credentialing process.
The Legacy Advantage: Why Outsource Your Credentialing?
Legacy's credentialing services positively impact your practice in the following ways:
🚀 Faster Provider Onboarding: Your new providers can start seeing patients and billing claims sooner, reducing revenue loss due to credentialing delays.
💰 Improved Cash Flow: With quicker enrollments, your practice can bill payors faster, preventing cash flow disruptions and ensuring steady revenue.
⏳ Less Administrative Burden: We take credentialing off your plate, allowing your staff to focus on patient care and operations rather than paperwork.
📈 Stronger Payor Relationships: Our team's expertise in working with insurance companies ensures smoother interactions and better outcomes for your practice. off your plate, allowing your staff to focus on patient care and operations rather than paperwork.
Clear & Transparent Pricing
We offer flexible pricing models to fit your practice's needs:
- Flat Fee: For straightforward credentialing services.
- Per Provider: This is typically for practices with multiple providers requiring individual credentialing.
- Hourly Rate: For complex credentialing needs, such as special payor enrollment or intricate situations.
Frequently Asked Questions
Case Study: Faster Billing, Better Cash Flow
Challenge
A 20-provider practice faced months-long delays in credentialing new hires, costing over $250K in lost billing opportunities.
Solution
Legacy Consulting implemented a credentialing tracker, facilitated CAQH updates, and direct follow-ups with payors.
Results
✔️ Reduced credentialing turnaround from 120 to 65 days
✔️ Restored $250K+ in collectible revenue
Featured Articles
Credentialing Services
Credentialing is a key piece to any practice or hospital. If providers are not properly credentialed, they will not be paid for their services. Credentialing is a long, comprehensive process that requires consistent follow up […]
Read MoreCredentialing and CAQH Completion
One of the most important pieces to opening a new practice, or moving from one practice to another, is your payor Credentialing. This is a time intensive process most providers or office managers do not […]
Read MoreService Spotlight: Credentialing
What exactly is physician credentialing? Essentially it is a payor’s way of ensuring that the provider has met all necessary qualifications to practice and is providing the appropriate level of care to their patients. While not […]
Read MoreGet Started with Legacy
Ready to simplify your credentialing process and bill sooner?
Let's Get You Credentialed - The Right Way, The First Time!
Stop losing valuable time and revenue - Partner with Legacy Consulting Services and experience a faster, smoother provider enrollment process.
Contact us for a free consultation to learn how we can simplify your practice's credentialing process and improve your cash flow or even assist with medical billing challenges.
For more helpful content and insider tips, please visit our blog.
About Legacy Consulting Services
Legacy Consulting Services is a healthcare consulting firm specializing in medical billing, provider credentialing, payor contracting, billing integrity audits, and revenue cycle optimization.
Core Values: Precision. Performance. Profitability.